Actual clinical settings where ECM systems were applied
In our previous posts, we summarized what types of Electronic Compliance Monitoring (ECM) Systems exist, and showed their strengths and weaknesses. Now we show some actual clinical settings where ECM systems were applied.
ECM and data volumes
The main advantage of ECM systems is that they can monitor hand hygiene compliance 24/7, and can gather plenty of data. Marra et al. 2010 compared direct observation with compliance measured by electronic dispenser counter. They found that direct observation can only monitor 1.3% of the hand hygiene events [1]. In McCalla et al. 2017 survey human observers collected 480 hand hygiene events, while their alcohol sensor-based monitoring system (Biovigil) captured 632,404 events [2]. Dai et al. 2015 published a multicenter survey about the impact of time at work and time off from work on hand hygiene compliance. For evaluation, they involved 4,157 health-care workers from 35 different hospitals, where an electronic dispenser monitoring system (nGage) was used. The use of this ECM system allowed them to analyze 13,7 million hand hygiene opportunities [3].
Direct observation vs. ECM systems
Some studies tried to compare the results of direct observation and ECM system data. Filho et al. 2014 compared data from a dispenser counter system (i-Healthsys) with data from direct observation, and found 92% accuracy [4].
Some survey found that ECM systems slightly underestimates compliance. Cheng et al. 2011 used MedSense system, and found that the system reports 14% less compliance than human observers [5, 6]. Swoboda et al. 2004 found that the electronic compliance rates were consistently 20% lower than simultaneously directly observed compliance rates [7, 8]. Fisher et al. 2013 found that their ECM system (HanGenix) measure 10% lower compliance rate, than human observers [9]. Filho et al. 2014 carried out continuous observation with ECM system, and also direct observation for a shorter period. They explained their results with the Hawthorne effect [4].
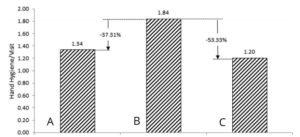
Figure 1.: Demonstration of the Hawthorne effect during hand hygiene observation: A: 1 hour before direct observation, B: during direct observation, C: 1 hour after direct observation. Compliance data was recorded by ECM system
(Source: Filho et al. 2014)
Accuracy of ECM systems
Most electronic systems only measure compliance at room entry and exit (Moments #1 and #4 from WHO My 5 moments of hand hygiene), entirely missing opportunities that occur inside the room. Unfortunately, most direct observations are also conducted this way. According to some estimations, monitoring only the entry and exit to/from the patient zone captures 80–85% of HH opportunities [8]. Sahud et al. 2012 claimed based on 378 direct observations that 8% of room entries did not include contact with a patient or his environment [10, 8].
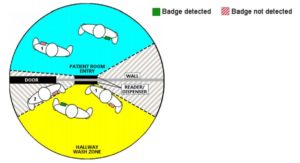
Pineles et al. 2014 installed a dispenser counter system (nGage), and while during the validation period, where they used simulated settings, the system worked almost perfectly, later, during the real-life clinical settings, when health-care workers were not instructed to modify their behaviors in any way. The performance of the system dropped: on room entry, 54.3%, and on room exits 49.5% were accurately recorded. The success of detection was mainly depended on the location of the reader, the health-care worker and the badge [11].
Does ECM systems increase hand hygiene compliance?
Most of the studies agreed that the use of ECMS can increase hand hygiene compliance. Michael et al. 2017 investigated two units at a tertiary medical center, Cleveland, OH. Hand hygiene compliance was measured by direct observation prior the application of the ECM system (Biovigil), an also after. Baseline hand hygiene compliance was 54% in the first unit and 52% in the second. During the application of ECM system compliance increased to 98% and 97%, respectively, and remained >80% even one year after the intervention [12].
Haidegger et al. 2016 described, that continuous monitoring with a hand hygiene technique monitoring device (Semmelweis Scanner) improve hand hygiene technique [13].
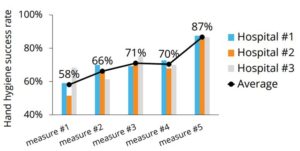 Figure 3: Effect of continuous monitoring on hand hygiene technique (Source: Haidegger et al. 2016)
Figure 3: Effect of continuous monitoring on hand hygiene technique (Source: Haidegger et al. 2016)
Does ECMS decrease HAI?
Unfortunately, there are limited data on this topic. McCalla et al. 2017 found, that during the period ECM system was in use more types of HAI dropped, but the reductions were not significant in any case [2].
Applying a dispenser-based ECM system (nGage) for a 7-month trial period, a medical center reported a decrease of 159 patient days and reduced hospital net losses of over $133,386, reflected on just 2,652 patient admissions [14].
Role of immediate feedback
Many studies confirmed that immediate, automated feedback is needed to increase hand hygiene compliance [2]. According to Michael et al. 2017, ECM systems with embedded feedback should be designed to stimulate behavior change [12]. Storey et al. 2014 claims, that immediate feedback was effective in increasing hand hygiene compliance, but feedback given retrospectively did not prevent a decrease in compliance [15]. Haidegger et al. 2016 proved that visualization and direct feedback on the quality of hand rubbing (Semmelweis Scanner) can be used efficiently to acquire the skills for proper hand hygiene [13].
Conclusion:
Electronic Compliance Monitoring System can record an enormous amount of data on a quite reliable way. Location-based ECM systems allow us to objectively monitor hand hygiene event compliance while technique monitoring systems can monitor the quality of hand hygiene. Several studies confirmed, that ECM systems can help to improve hand hygiene, but there are only limited data on how they reduce HAI. Immediate, automated feedback help sustain high compliance.
Read our previous post about the Electronic Compliance Monitoring Systems. Please stand by for our next blog entry on the cost of the ECM systems.