Who was he & why are we so proud of his legacy?
The Semmelweis Scanner was named in honor of the Hungarian physician, Ignaz Semmelweis. Now, giving you a brief summary who he was, and why we are so proud of his legacy.
Ignaz Semmelweis was born in 1818, Budapest, Hungary (then part of the Austro-Hungarian Empire) [1]. After finishing his schooling at the University of Pest, he travelled to Vienna to start a law school. Soon after his arrival, he became so attracted to medicine that he decided to change to medical school. Vienna Medical School was already one of the world leading centers at that time. He received Master’s degree in practical midwifery, and also learned diagnostic and statistical methods [2].
In 1846, he started to work at the Vienna General Hospital, and was faced with the most pressing problem; the high maternal mortality rate due to puerperal fever (childbed fever). At that time, most women delivered at home, but those who needed hospitalization faced mortality rates up to 20%. The cause of puerperal fever was not known, some thought that it was caused by overcrowding, poor ventilation, the onset of lactation, or miasma [1].
Semmelweis observed that the mortality rate was different in the two divisions of the hospital; 16% at Division 1 and only 7% at Division 2 [3]. He concluded, that the higher mortality rates in Division 1 must had been due to a factor that was unique to that ward. A main difference between the clinics was staffing; care was administered by obstetricians and medical students in Division 1 and midwives in Division 2 [4].
 Ignaz Semmelweis (1818-1865)
Ignaz Semmelweis (1818-1865)
In 1847, one of his friends, Jacob Kolletschka, a professor of forensic medicine died tragically after his finger was punctured with a knife during an autopsy [2]. This febrile illness had very similar symptoms to puerperal fever. To Semmelweis, the one factor that was common to the women of Division 1 and Kolletschka, and that differentiated them from Division 2, was exposure to so called “cadaverous particles”. He hypothesized that puerperal fever was an infectious disease, it was transmitted from dissecting room to patients by healthcare workers’ hands [4].
He noticed that hands have a strange odor after autopsy, but the smell disappears after washing hand in chlorinated lime solution. Although Semmelweis did not understand the process – it was more than two decades before the germ theory was born – he ordered that staff and students must wash their hands with chlorinated lime solution before each examination. Under these procedures, the mortality rate dropped from 18% to 1.3% in Division 1 [1].
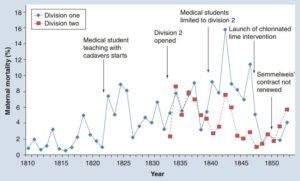
Figure 1: Maternal mortality rates at the Vienna General Hospital (Allgemeines Krankenhaus) from 1810 until 1852 [4].
In 1848, a political revolution swept across Europe, and Semmelweis took part in the events in Vienna. After the crush of the revolution in 1849, he was dismissed from his post. He only found an unpaid instructorship in midwifery. During this time, he started to carry out animal experiments with Erns Brücke, to validate the clinical conclusions [2].
In 1850, he decided to return to Budapest and started to work at the St. Rochus Hospital. An epidemic of puerperal fever had broken out in the obstetrics department. At his request, Semmelweis was put in charge of the department. He repeated the same intervention; the chlorinated lime hand washing [4]. The mortality rate reduced promptly to 0.85%, while in the meantime, in Prague and Vienna the rate was still 10–15% [1].
In 1855, he became appointed professor of obstetrics at the University of Pest (today’s Semmelweis University) [1]. His lectures attracted large student audiences [2]. He published his findings in 1861, titled The Etiology, Concept, and Prophylaxis of Childbed Fever (Die Ätiologie, der Begriff und die Prophylaxis des Kindbettfiebers). He sent it to all opinion leaders and medical societies, but the general reaction was negligence [1].
In 1865, he suffered from conditions what appeared to be a form of mental illness, and was taken to a mental hospital in Vienna, where he died. Ironically, his death was caused by the infection of a wound. He died of the same disease against which he had struggled all his professional life [1, 2].
Semmelweis is recognized as one of the greatest physicians to live, he is part of the UNESCO World Cultural Heritage. Today, a prestigious university, streets, institutes, a foundation and a conference series bear his name.
Conclusion:
Ignaz Semmelweis introduced antisepsis into medical practice a quarter of a century before Pasteur and Lister developed the germ theory and surgical antisepsis. He was also a pioneer of evidence-based medicine, as his based theory on strong statistical evidence. He used a “built-in control group” of women at the Division 2, a fortunate situation unparalleled elsewhere [2]. He was the first to introduce a targeted system change involving hand hygiene to successfully fight against infections [4]. Therefore, Semmelweis is considered to be not only the father of hand hygiene, but his intervention is also a model of epidemiologically driven strategies to prevent infection [3].
Read our previous post about the first Semmelweis CEE conference on Hospital Hygiene and Patient Safety. Please stand by for our next blog entry on a summary of the second Semmelweis CEE conference, held this week.