8 Proven Ways to Lower Your SSI Rates by Rebecca Rudolph
Surgical site infections (SSIs) are the second most common healthcare-associated infection (HAI), and colorectal surgery patients are at a disproportionately higher risk for getting them. In an effort to figure out why and how to lower SSI rates, the American College of Surgeons, Joint Commission Center for Transforming Healthcare and seven healthcare facilities partnered to do a two-and-a-half year study. This data was presented in a July 21 symposium by the Joint Commission, Medline and Cleveland Clinic, which was a study participant.
“The results of the project show that surgical site infections are a complex problem with a number of contributing factors that vary by organization,” said Coleen Smith, high reliability initiatives director for the Joint Commission. “No two organizations will likely have the same set of contributing factors indicating that the solutions they implement will also be different.”
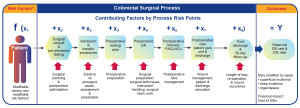
The study evaluated various contributing factors to SSIs, such as patient characteristics, surgical procedure, perioperative and intraoperative process, postoperative process and measurement challenges. As information was collected, facilities implemented improvement solutions – sometimes all at once and sometimes one at a time. They said the following helped drive success:
-
Emphasis on the use of data to guide and drive improvement decisions and implementations
- Sharing real-time data with all staff who care for colorectal surgical patients
- A committed colorectal surgeon champion who led the project
- A dedicated core team that included front-line staff from each process area and subject matter experts
- Continuous engagement of the core team throughout the project
- Leadership ensured that surgeons and other staff who worked on the project received needed support, including dedicating a certain amount of time to the project
- Engagement of staff and patient/caregivers, giving a voice to both internal and external customers
- An organizational culture that held everyone accountable for preventing the occurrence of SSIs. This sense of accountability was pervasive, reaching every touch point in every surgical patient’s journey – from pre-admission, to preoperative, to the OR and PACU, through to the patient care unit and post discharge care.
 (Courtesy of the Joint Commission)
(Courtesy of the Joint Commission)
“The solutions are validated by the original project teams to assure that they are feasible to implement,” Smith said. “In fact, they are further tested and validated in additional pilot testing. The improvements implemented by the organizations are not only effective, they are also efficient, because organizations are not implementing solutions for problems they do not have.”
The seven participating facilities saw an overall 45 percent reduction in incisional SSIs, and a 32 percent reduction in colorectal SSIs. They associated the estimated 135 prevented infections with a cost savings of more than $3.7 million. The average length of patients stay also decreased from 15 days to 13 days.
 (Courtesy of the Joint Commission)
(Courtesy of the Joint Commission)
“The surgical team is, of course, an integral part of the patient care team and, therefore, of the project team,” Smith said. “Getting their buy in for the project and the solutions is crucial to sustaining the improvements that resulted in reduced SSI rates.”
Researchers think if the methods, solutions and lessons learned through this study are implemented, about 30,420 colorectal surgery infections can be prevented, which could save up to $834 million. The Joint Commission plans to develop this study data into a web-based application called the Targeted Solutions Tool.
Source: www.surgicalprodutcsmag.com