Can healthcare-workers (HCW) wear artificial nails at work? Can they use nail polish? How long their nails should be? What do guidelines say, and what are the scientific evidences?
In this post – as in our recent posts about rings and watches – we are only talking about hand hygiene during regular patient care. It is relatively clear that in case of surgical hand rubbing, stricter rules must apply to artificial nails, nail polish and long nails [1].
Several studies claim that the subungual areas of fingers harbor high concentration of bacteria, even after careful hand hygiene. These bacteria are most frequently coagulase-negative staphylococci, Gram-negative rods and yeasts.
Long and in particular, sharp nails can puncture gloves, and can deteriorate the hand hygiene performance [1]. HCW may try to protect their nail art from damage by reducing hand hygiene [2].
ARTIFICIAL NAILS
Artificial nails are an important risk factor. HCW who wear it are more likely to harbor Gram-negative pathogens [1]. CDC guideline says that it is unknown, whether artificial nails contribute to pathogen transmission, therefore CDC only suggests to remove artificial nails when having contact with high risk patients, e.g., in an intensive-care unit [3]. In contrast, the WHO guideline says that HCW cannot wear artificial nails. Percentage of HCW who wear artificial nails against the recommendation is a performance indicator, that can be monitored regularly (e.g., bi-annually).
In a self-administered survey in a NICU, 8% of staff reported to wear artificial fingernails, and 61% believed that removing artificial fingernails would reduce the risk of infections. Only 47% thought that a policy prohibiting the use of artificial nails would help to reduce infections, even so 74% claimed that they would remove artificial fingernails, if it was recommended [4].
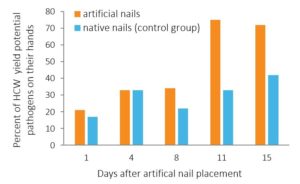
Hedderwick et al. 2000 isolated pathogens from HCW’s hands more frequently when they wore artificial nails then in the case of native nails (92% and 62%, respectively). They also found that the longer the artificial nails were worn, the more likely a pathogen was isolated [5].
Figure 1: Nail colonization by potential pathogen organisms increase over time.
Source: Hedderwick et al. 2000
Many outbreak investigations found that wearing artificial nails plays a role in infections caused by Gram-negative bacilli or yeast [1]. A Klebsiella pneumoniae outbreak investigation in a neonatal intensive care unit (NICU) found that exposure to a HCW who wore artificial nails were associated (odds ratio, OR=7.87) with infection and colonization [6]. In another case, Serratia marcescens bacteremia in a hemodialysis center were associated with a nurse who wore artificial fingernails upon openingheparin vials [7]. In a NICU, 10% of neonates acquired Pseudomonas aeruginosa bloodstream infection, and 35% of the infected babies died. During the outbreak investigation, 104 HCW’s hand cultures were examined. P. aureginosa was found only on three nurses’ hands, and multivariate logistic regression analysis showed that colonization was associated with two of those three nurses. One of them wore artificial nails, while the other had long natural nails [8].
NAIL POLISH
In some studies, there were no significant changes in hand microbiology when nail polish was used, while other studies found that hand contains more bacteria, if nails were polished [9, 10] WHO and CDC guidelines attempt to resolve the contradiction, and claim that freshly applied nail polish does not increase the bacterial load of the hands, while chipped nail polish can accumulate a higher number of bacteria [1, 3]. According to the National Health Services (NHS) in the UK, HCW should refrain from using nail polish [11].
LENGTH OF NAILS
The NHS guideline says that nails must be short, but it is not defined what “short” means exactly [11]. WHO and CDC guideline both say that nails should be shorter than 0.5 cm or ¼ inch [1]. However, the CDC guideline and the guideline of Public Health Agency of Canada both remark that the majority of bacteria grows along the proximal 1 mm of the nail adjacent to subungual skin, hence it is unknown whether the length of nails is really a significant risk factor [3].
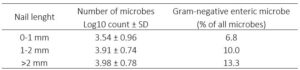
Rupp et al. 2008 investigated hand culture of 69 nurses working in an ICU. They found increased number of microbes, and the increased number of microbe species were associated with more than 2 mm long nails [12].
Table 1: Microbiological flora of HCW. Source: Rupp et al. 2008
Another study examined HCW’s hand microbiology, and they found that if nails were longer than 2 mm, hand were more likely contaminated with Staphylococcus aureus (OR=2.17) [10]. Based on these two investigations, Fagernes et al. 2011 recommended that fingernails should not be no longer than 2 mm.
Very few HCW have long native nails, while artificial nails are long and polished. Therefore, in most studies, it is difficult to tell whether the increase of colonization was caused by the length of the nails, the nail polish, or the artificial nails [5].
CONCLUSION:
WHO hand hygiene guideline concludes that each healthcare facility should have a policy about artificial fingernails and nail polish use. Wearing artificial nails, using nail polish, or having long native nails all can be a risk factor. Although not every national/international guideline prohibits them, patient safety can be improved if HCW have short, native, unpolished nails.
Read our previous posts on wearing rings or watches during patient care.