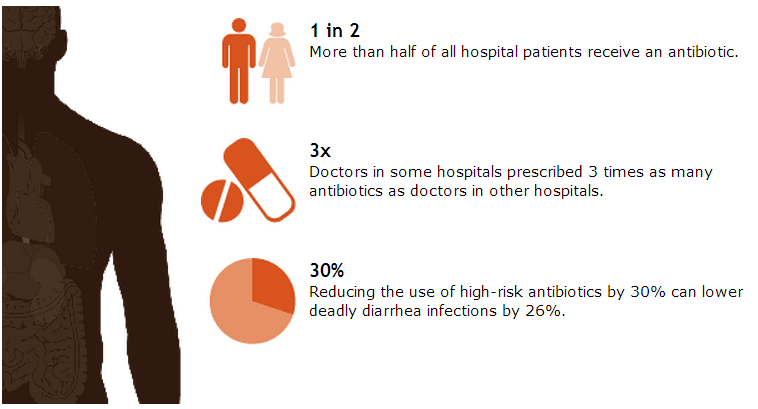
Antibiotics save lives, but poor prescribing practices are putting patients at unnecessary risk for preventable allergic reactions, super-resistant infections, and deadly diarrhea. Errors in prescribing decisions also contribute to antibiotic resistance, making these drugs less likely to work in the future.
A CDC report found that, in hospitals, a 30 percent reduction in use of the antibiotics that most often cause deadly diarrheal infections withClostridium difficile can reduce these infections by more than 25 percent. The same antibiotics also prime patients for future super-resistant infections.
To help hospital develop antibiotic prescribing improvement programs (also called “antibiotic stewardship” programs), CDC released practical tools that include seven key elements, a self-assessment checklist, and an in-depth implementation document. The stewardship program of each hospital should include seven core elements:
- Leadership commitment: Dedicate the necessary human, financial, and IT resources.
- Accountability: Appoint a single leader responsible for program outcomes. Physicians have proven successful in this role.
- Drug expertise: Appoint a single pharmacist leader to support improved prescribing.
- Act: Take at least one prescribing improvement action, such as requiring reassessment of prescriptions within 48 hours to check drug choice, dose, and duration.
- Track: Monitor prescribing and antibiotic resistance patterns.
- Report: Regularly report prescribing and resistance information to clinicians.
- Educate: Offer education about antibiotic resistance and improving prescribing practices.
It is also critical to work with other health care facilities in the area to prevent infections, transmission, and resistance.