When to wear and when to remove?
The use of examination gloves during patient care can reduce the risk of contaminating healthcare workers’ (HCW) hand with pathogens, and reduce the chance of pathogen dissemination. Controversially, gloves represent a risk for pathogen transmission and infection if used inappropriately [1]. What should we keep in mind when wearing gloves?
According to the WHO, there are 3 major indications for glove usage:
- contact with blood or other body fluids
- touching patient during contact precautions
- before sterile condition
Each step protects both the patient and the HCW. In the first two cases, gloves prevent the gross contamination of HCW’s hands. It is important, because handwashing or hand antisepsis after procedures may not remove all potential pathogens when hands are heavily contaminated, it only can reduce its number and may pose a hazard even with the reduced number of pathogens (e.g., the ASTM E-1174 standard require 2-3 log10 reduction).
Glove should be removed, if
- the glove is damaged
- contact with blood, body fluid, mucous membrane has ended
- contact with a contaminated body site on a patient ended
- there is an indication of hand hygiene
Gloves are far from perfect. Pathogens can gain access through gloves to the hands via small defects on gloves or during the glove removal, if it is performed incorrectly. The pathogen colonizing the patient may be recovered from 30% of HWC’s hand, although they wore gloves during patient contact [1]. Another study found that 5–10% of HCW’s hands were contaminated after glove removal [2, 3].
Therefore, HCW should perform hand hygiene before donning gloves and after doffing it. According to the WHO recommendation, gloves must be removed and hand hygiene must be performed when a new, not contaminated body site is treated within the same patient. Glove usage cannot replace hand hygiene or anyhow modify hand hygiene indications, so hand hygiene must be performed according to the well-established 5 moments of hand hygiene [1]. Additionally, as we previously discussed, putting gloves on hand still wet of a handrub can cause skin problems. It is a challenge, but it is absolutely necessary to combine hand hygiene and glove use.
Chau et al. 2011 observed 304 glove using episode, and found that only 25% of participants changed gloves between procedures on the same patients (Table 1.), this was the major breach of compliance [4].
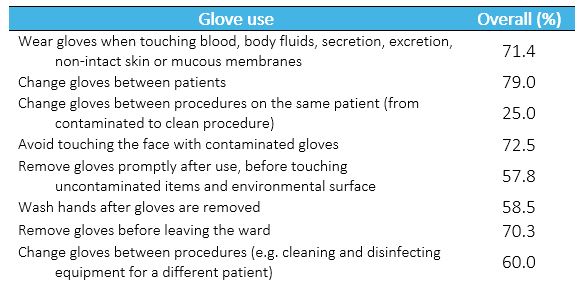
Table 1. Performance in glove use (based on 304 episodes). Source: Chau et al. 2011
Loveday et al. 2016 observed 163 glove-uses, and found that glove use was inappropriate in 42% of episodes. The risk of cross-contamination was mostly associated with not removing the gloves or not performing hand hygiene after. Hand hygiene was performed 61% before gloves were put on, and 68% after glove removal [5]. Squeri et al. 2016 found that HCW did not change gloves in 64% of cases before caring for a new patient [6]. Paramedics in a survey said that 58% of them only changed their gloves at the end of the case [7].
According to Pan et al. 2007 donning glove was “a self-protective practice, rather than as a practice that reduces the risk of cross-transmission” [8]. Another study described that HCW put on gloves before entering an isolated patient’s room, and only remove it after leaving the room. It seems that there is also a psychological component; the belief that wearing gloves can replace hand hygiene [7].
In an Intensive Care Unit (ICU) two 3-month-long periods were compared. First period were “standard practice”, second period was “universal gloving”, when HCW had to wear gloves before every patient contact. Actual glove wearing was 32% during period 1, and rose to 87% during period 2. At the same time, hand hygiene decreased, and infection rates increased, as shown in Table 2 [9].
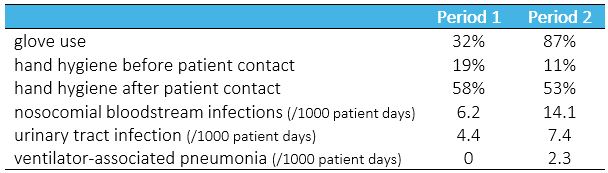
Table 2: Compliance with infection control practices and nosocomial infection rates. Source: Bearman et al. 2007
One reason of relatively low compliance can be that adherence to the protocol is really time consuming. Let us imagine a nurse who has to measuring blood pressure, and after drawing blood from a patient. This require 3 or 4 hand hygiene events (before touching patient, before donning glove, after glove removing and after touching patient environment, if it happened), each should take at least 20–30 seconds.
Loveday et al. 2016 made interviews with HCW about gloves usage. One of them answered “I use the Alcogel (ABHR) on the gloves…. and I start a new procedure, obviously, it’s not aseptic but …” Decontamination of gloved hand can be a realistic alternative. This practice seems to be wide spread, despite of the warning by the WHO that ABHR may dissolve the glove material [1]. In 2016, the Robert Koch Institute (Germany) stated that disinfection of gloved hand can be acceptable, if the workflow can only be assured without changing glove. Some studies already confirm, that disinfection of gloved hand is as effective, as on bare hands [7]. Gloves are labeled as a single use product, “intended for one use, or for use on a single patient during a single procedure”. Reusing gloves is also a legal issue [10].
Conclusion:
There are clear recommendations on when gloves should be put on and remove. Wearing gloves cannot substitute proper hand hygiene, and hand hygiene must also be performed before donning glove and after doffing it. Complying with all the recommendations is time consuming and in many case unrealistic, while noncomplying can contribute to pathogen transmission. Decontamination of gloved hand can be a possible solution, but most of the protocols do not support it, as it need further evaluation.
Read our previous post on when should we perform hand hygiene, and how to avoid skin irritation.