- Why are repeated hand hygiene trainings mandatory?
- How big is the problem of skill retention?
One of our major clinical studies (Lehotsky et al. 2015) aimed to answer these questions.
But before describing that, let’s summarize what we know about the frequently missed areas in hand hygiene.
Taylor 1978 examined the hand surface coverage during hand hygiene with alcohol and found that 89% missed some parts of their hands. Missed parts were usually the thumbs and fingertips.
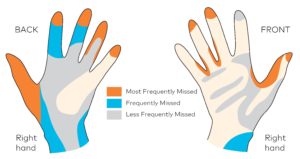
Figure 1: Distribution of areas inadequately treated during hand washing in Taylor 1978 paper.
Ayliffe 1978 described a procedure; a step-by-step guideline how to perform hand hygiene to reach complete coverage. This method consists of five strokes forwards and backwards in 6 different positions. It paid special attention to thumbs (step5) and fingertips (step6). In Bellamy 1993, the 6-step guideline is first referred to as a standard procedure. The 6-step became the base of the EN 1500 regulation about the efficacy validation of hygienic hand rubs (first published in 1997, then updated in 2003 and in 2015) by the European Committee for Standardization. The same 6-step is the core element of the most widely known ‘How to handrub’ and ‘How to Handwash’ protocol released by the WHO in 2005.
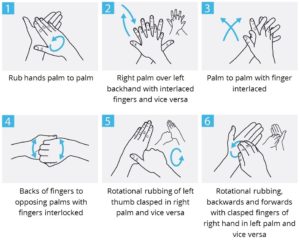
Figure 2: The 6-step from WHO ‘How to handrub’ and ‘How to handwash’ guide.
In Ayliffe 1978 it was mentioned that wrists also need to be rubbed. Many hospitals use a 7-step hand rubbing protocol where the 7th step is rubbing the wrists worldwide.
Our study in short
The focus of the study was to investigate the change in hand hygiene technique of healthcare workers (HCW) over time. Hand hygiene effectiveness was measured by the Semmelweis Scanner, and immediate, objective visual feedback was provided to each user. Using the fluorescent method, the number of insufficiently disinfected areas were identified on the hand surface. Hand hygiene technique was considered ‘wrong’ if more than 3 areas were missed, or ‘inaccurate’, if there were 1–3 missed areas on HCW’s hand. In the case of ‘perfect’ technique, hands were fully covered by the handrub [1].
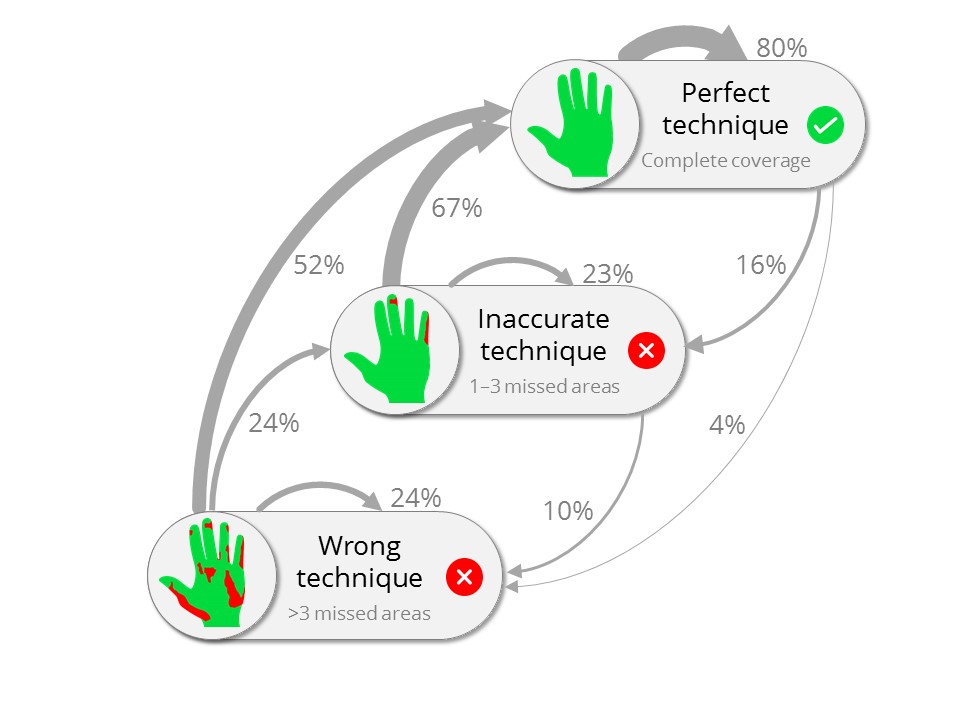
Figure 3: Effect of repeated feedback on healthcare workers’ hand hygiene technique.
Methodology and Findings
136 HCW from 3 European hospitals were involved in the study. As presented in Figure 3, if the previous hand hygiene event was inaccurate after providing objective feedback with the Semmelweis Scanner, there is 67% probability that the next hand hygiene event will be flawless. This means natural learning based on our mistakes. There is a 23% probability that the repeated hand hygiene technique will stay inaccurate, and a slight chance (10%) that it will become worse. A ‘perfect technique’ event is 80% likely to be followed by another ‘perfect technique’ event, but there is 20% probability that the previously perfect technique falls behind [1]. This is the phenomenon called skill retention, meaning that a previously acquired skill is maintained through time [2].
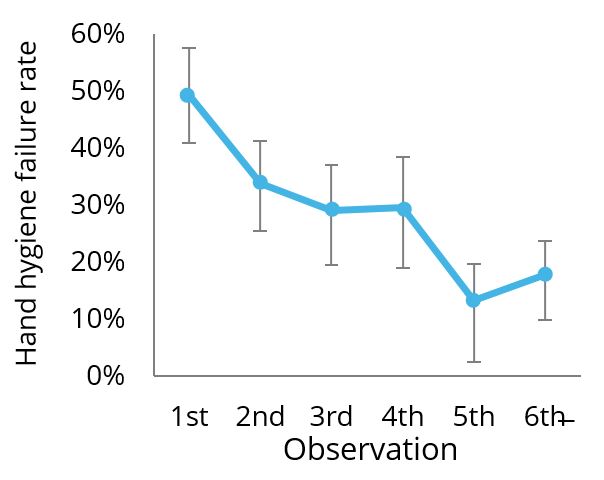
Figure 4: Effect of continuous monitoring and immediate feedback on hand hygiene technique.
The study also investigated how repetitive feedback changes hand hygiene performance. Figure 4 shows that hand hygiene failure rate (either inaccurate or wrong technique) dropped significantly; from the initial 49.3% to 13.3% by the fifth observation, confirming that repetitive feedback can improve hand hygiene technique [1].
Conclusion
Direct feedback on hand hygiene technique by the Semmelweis Scanner improves hand hygiene over time. Skill retention is threatening important issue, calling for continuous training to improve and maintain hand hygiene. The constant presence of a monitoring device in hospital wards could be beneficial in this regard.