Should healthcare-workers (HCW) be allowed to wear rings during patient care? What do guidelines say, and what scientific evidence exists?
It is indisputable that rings (and all other jewelry) must be removed before surgical hand preparation, and cannot be worn in the Operating Room. In theory, it should be the same in the case of routine patient care and hand rubbing, but the practical situation is not so clear.
Having reviewed the literature, the CDC 2002 hand hygiene guideline concluded that it is unknown whether wearing rings results in greater transmission of pathogens, and further studies are needed [1]. The WHO guideline (published in 2009) is in a position: “strongly discourage the wearing of rings or other jewelry during health care”. Although it also mentions that a “simple wedding ring (band) during routine care may be acceptable”, recognizing religious and cultural aspects by that [2].
Many studies agree that wearing a ring have a negative effect on hand rubbing. Hautemaniere et al. 2010 examined the hand hygiene technique by direct observation, applying the fluorescent method. Hand hygiene was considered effective if the uncovered skin area was smaller than 7%. In this study, rings other than a wedding ring were associated with significantly lower effectiveness of hand rubbing. In the case of a plain (no stone, no structural element) wedding ring, the negative effect was not significant [3]. When interpreting these results, we should keep in mind that hand hygiene was considered ineffective despite complete coverage if rubbing time or prescribed method were not respected. As Trick et. al 2003 pointed out, “it is possible that nurses who wore rings were less likely to adhere to infection-control practices” [4].
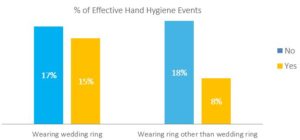
Figure 1: Impact of rings on the effectiveness of hand hygiene. Data from Hautemaniere et al. 2010
Ramón-Cantón et al. 2011 described that 18% of HCW wore one or more rings according to their observation. The effectiveness of hand rubbing was examined using the fluorescent technique. 84.3% of those wearing one or more rings had missed areas on fingers, compared to 46.3% of those who did not wear any [5].
Trick et. al 2003 studied risk factors for hand contamination. The gloves juice method was applied for microbiological sampling. Ring wearing was found to be a risk factor for hand contamination, and risk was even higher when more than one ring was worn (odds ratio [OR] for one ring: 2.6, OR for >1 ring: 4.6). 22% of participants worn rings at home and removed it at work, 24% worn rings both at home and at work. Wearing rings only at home was not determined as a risk factor [4].
Yildirim et al. 2008 compared colony counts on nurses’ hands providing direct patient care in intensive care units. Wearing rings was associated with elevated bacterial colonization after using handrub; both Gram-negative and Gram-positive colonies were significantly higher in numbers. They did not find difference between plain wedding rings and rings with stones. In this study, all examined rings were of 14 or 18 karat gold [6].
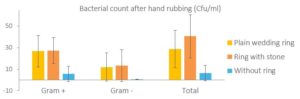
Figure 2: Impact of rings on the bacterial load of hands. Data from Yildirim et al. 2008
Khodavaisy et al. 2011 investigated HCW’s hand and their rings separately during their routine work in an ICU. Microbiological sample was collected by sterile swabs, both form hand and ring surfaces. 86.9% of HCW who wore ring had bacterial or fungal contamination on their hands; in contrast, 28.7% of HCW without ring. Several microorganisms were found on rings, such as Staphilococci (28%), Candida (15%), Aspergillus (13%), E. coli (11%), Rhodotorula (9%), Klebsiella (7%), Enterobacter (4%), Acinetobacter (4%). Most of isolates are known to cause nosocomial infections [7].
Fagernes et al. 2009 examined how rings impact the transmission of bacteria. Participants shook hands with the investigator who wore sterile glove. After this episode, microbiological sample was collected from investigator’s glove and from HCW’s bare hands. Bacterial load was significantly higher (OR 2.63) on ringed hands, and significantly higher number of bacteria were transmitted (OR 2.43) [8].
Some studies claim that ring wearing does not have negative influence. Wongworawat et al. 2007 compared bacterial count on ringed and plain hands with the glove juice technique after hand rubbing, and did not find significant difference [9]. Fageners et al. 2007 described that a single, plain ring did not increase the total bacterial load; however, it was associated with an increased rate of Enterobacteriaceae carriage [10].
CONCLUSION:
The practices of ring wearing are a bit controversial, but most of the studies found that it has a negative effect on hand hygiene. Taking off rings during patient care is a really simple “intervention” that can contribute to improve patient safety.
Continue reading: Hand Hygiene and Rings – Part 2
Read our previous posts on the fluorescent trial, how to handrub