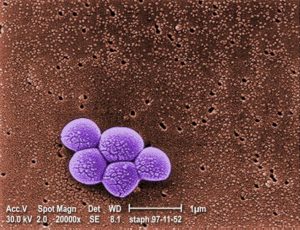
What is MRSA?
Staphylococcus aureus is a gram-positive bacterium, the one of the main causes of hospital-acquired infections (HAI), responsible for 15% of all HAI [1] Before the use of antibiotics, S. aureus infection was often fatal. Even in the early 1940s, mortality was as high as 82% [2]. Antibiotic resistant S. aureus strains are a significant threat for the healthcare system even today. MRSA, the Methicillin Resistant Staphylococcus aureus is one of the most common antibiotic resistant pathogens.
 Image: CDC, Melissa Dankel 2014
Image: CDC, Melissa Dankel 2014
How much an MRSA infection cost for the hospital?
There are several different estimations, how much an MRSA infection costs. Here are some example from the studies:
| Reference | Study settings | MRSA cost | Extra hospital days |
| Ben-David 2009 [3] | Hospital in Rhode Island, ICU, bloodstream infections (BSI) | $114 000 | 20 days |
| Cummings 2010 [4] | 750-bed medical center in North Carolina | $47–53 000 | – |
| Filice 2010 [5] | Veterans Affairs hospital | $34 000 | – |
| Rubio-Terrés 2010 [6] | 27 hospitals in Spain | €11 000 | 25 days |
| Stewardson 2015 [7] | 10 European hospitals, BSI | €11 000 | 12 days |
| WHO [8] | $20–114 000 | – |
High hospital costs resulted from longer antibiotic treatment, additional tests, longer hospital stay, and higher rate of ICU admission, and a significantly higher rate of readmission. MSRA infected patients need to be isolated, while isolation results in further elevated costs.
In the USA, there are 120 000 hospitalizations annually with MRSA infection, and direct medical cost is estimated at $27-35 000/patient. In the UK, the NHS has over £3 billion/year expenses only due to MRSA-caused additional hospital stay. [9]
How can we prevent MRSA infections?
CDC, SHEA and WHO have detailed recommendations for MRSA control. According to a most recent study, 91% of the US hospitals reported using some kind of MRSA prevention, including improved hand hygiene, active testing, isolation, environmental decontamination and education [10].
One of the most typical ways MRSA spreads in hospitals is via hand contact. Marimuthu 2014 [11] reported that a complex hand hygiene campaign increased hand hygiene compliance from 48% to 66%, and during this period, MRSA rate decreased from 0.74 to 0.24 / 10 000 patient days. In another study hand hygiene compliance increased from 41% to 87% and S. aureus bacteremia decreased from 2.1 to 1.4 / 10 000 patient days. In Singapore, the NUHS found that the MRSA bacteremia ratio went down from 2.6 to 1.1 / 10 000 patient days, while hand hygiene compliance increased from 47% to 69%. [12]
How much the MRSA prevention costs for the hospitals?
According to Cummings 2010 [4], a 200-bed hospital has ca. $1 800 000/year MRSA-related expenses, mostly because of hand hygiene non-compliance. A 1% increase in hand hygiene compliance results ca. $40 000 annual savings.
The Netherlands have an anti-MRSA policy called “Search and Destroy”. The University Hospital Maastricht during the 2000-2004 period spent €1 400 000 for searching MRSA, and another €2 700 000 for MRSA prevention and treatment. Nulens 2008 [13] claims that MRSA prevention costs are much lower than the costs of MRSA treating.
Conclusion:
Hand hygiene together with early detection and isolation are cost-efficient and effective counter-measures against MRSA. Stay safe!
Read more on how and when to perform hand hygiene