As part of WHO’s commitment to safety and protection of healthcare workers and patients from transmission of Ebola virus disease, WHO has conducted a formal review of personal protective equipment (PPE) guidelines for healthcare workers and is updating its guidelines in context of the current outbreak.The guidelines are based on a review of evidence of PPE use during care of suspected and confirmed Ebola virus disease patients. The Guidelines Development Group convened by WHO included participation of a wide range of experts from developed and developing countries, and international organizations including the United States Centers for Disease Control and Prevention, Médecins Sans Frontières, the Infection Control Africa Network and others.
“These guidelines hold an important role in clarifying effective personal protective equipment options that protect the safety of healthcare workers and patients from Ebola virus disease transmission,” says Edward Kelley, WHO Director for Service Delivery and Safety. “Paramount to the guidelines’ effectiveness is the inclusion of mandatory training on the putting on, taking off and decontaminating of PPE, followed by mentoring for all users before engaging in any clinical care.”
Guidelines were developed from an accelerated development process that meets WHO’s standards for scientific rigour and serves as a complement to the Interim infection prevention and control guidance for care of patients with suspected or confirmed filovirus haemorrhagic fever in health-care settings, with focus on Ebola, published by WHO in August 2014.
Use of the personal protective equipment
Experts agreed that it was most important to have PPE that protects the mucosae – mouth, nose and eyes – from contaminated droplets and fluids. Given that hands are known to transmit pathogens to other parts of the body, as well as to other individuals, hand hygiene and gloves are essential, both to protect the health worker and to prevent transmission to others. Face cover, protective foot wear, gowns or coveralls, and head cover were also considered essential to prevent transmission to healthcare workers.
“Although PPE is the most visible control used to prevent transmission, it is effective only if applied together with other controls including facilities for barrier nursing and work organization, water and sanitation, hand hygiene, and waste management,” says Marie-Paule Kieny, Assistant Director-General of Health Systems and Innovation. Benefits derived from PPE depend not only on choice of PPE, but also adherence to protocol on use of the equipment.
A fundamental principle guiding the selection of different types of PPE was the effort to strike a balance between the best possible protection against infection while allowing health workers to provide the best possible care to patients with maximum ease, dexterity, comfort and minimal heat-associated stress.
In this situation where evidence is still being collected, to see what works best and on an effective sustainable basis, it was considered prudent to provide options for selecting PPE. In most cases, there was no evidence to show that any one of the options recommended is superior to other options available for healthcare worker safety.
Further work is needed to gather scientific experience and data from the field in systematic studies, in order to understand why some health workers are infected in the current outbreak and to increase effective clinical care. WHO is committed to working with international partners on these issues to build this evidence base.
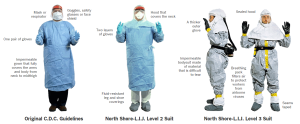
These protocols, some specified by the C.D.C., were in place at some hospitals when Mr. Duncan was being treated in Dallas.
Related posts: